Understanding Root Canals: What You Need to Know
A root canal is one of the most common dental procedures that people associate with pain and discomfort, but in reality, it’s designed to alleviate severe tooth pain and save a damaged tooth. Despite its somewhat fear-inducing reputation, a root canal is a routine and highly effective treatment that has helped millions of people preserve their natural teeth and avoid more invasive procedures, like extractions. In this article, we will dive into what a root canal is, why it’s necessary, how it’s performed, and the recovery process.
What is a Root Canal?
A root canal is a dental procedure used to treat infection at the center of a tooth (the root canal system). The center of each tooth contains a soft tissue known as pulp, which houses nerves, blood vessels, and connective tissue. If this pulp becomes damaged or infected, it can cause intense pain, swelling, and even tooth abscesses. The goal of a root canal is to remove the infected pulp, clean the inside of the tooth, and seal it to prevent future infection.
A root canal can be done on both front and back teeth, and it’s often necessary when a tooth has been deeply damaged by decay, injury, or repeated dental procedures. The treatment helps save the tooth and allows it to continue functioning normally.
Why Would You Need a Root Canal?
There are several reasons why you might need a root canal. Some of the most common causes include:
- Severe Tooth Decay: When tooth decay progresses deep into the tooth, it can reach the pulp and infect it. At this point, a root canal may be needed to remove the infected tissue and prevent further damage.
- Tooth Injury or Trauma: A cracked or broken tooth due to an accident, sports injury, or biting on something hard can expose the pulp to bacteria, leading to infection.
- Repeated Dental Procedures: Multiple fillings or treatments on the same tooth can cause the pulp to deteriorate over time, potentially leading to infection.
- Gum Disease: Advanced gum disease (periodontitis) can cause the pulp of a tooth to become infected, requiring a root canal.
- Abscessed Tooth: An abscess, or a pocket of pus, can form at the root of a tooth due to bacterial infection. If left untreated, an abscess can spread and lead to further complications.
Symptoms that indicate the need for a root canal include:
- Severe toothache or pressure
- Sensitivity to hot and cold that lingers after the stimulus is removed
- Swelling and tenderness in the surrounding gums
- Darkening or discoloration of the tooth
- A pimple-like bump on the gums near the tooth
The Root Canal Procedure
A root canal procedure is typically performed in one or two visits to a dentist or endodontist (a specialist in root canal treatments). Here’s a step-by-step breakdown of the process:
- Examination and X-rays: Before the procedure begins, your dentist will take X-rays to assess the extent of the infection and identify the root canals in the tooth. This helps the dentist plan the treatment.
- Anesthesia: Local anesthesia is administered to numb the tooth and surrounding area. While you may feel some pressure during the procedure, the goal is to ensure that you’re as comfortable and pain-free as possible.
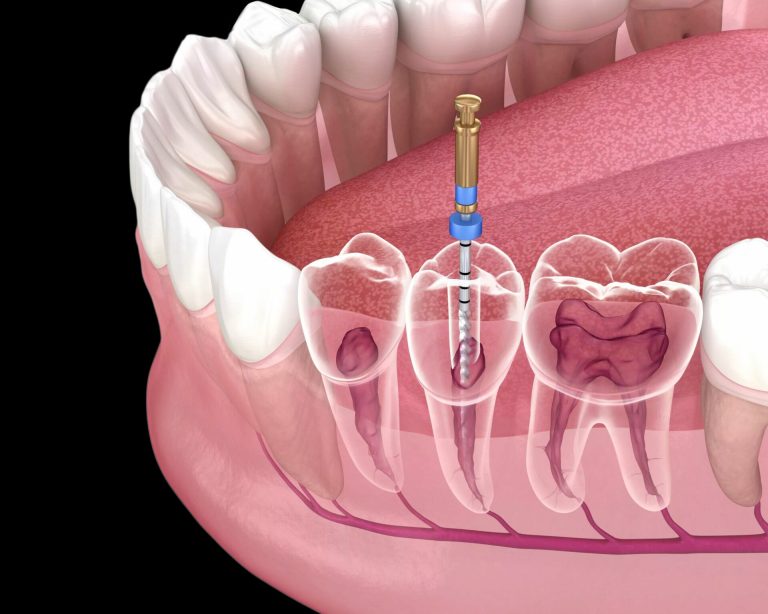
- Accessing the Pulp: The dentist will make a small opening in the crown (the top) of the tooth to access the pulp chamber. If the infection has caused the pulp to die, the dentist will remove it along with any decayed tissue.
- Cleaning and Shaping the Canal: Once the infected pulp is removed, the dentist will use special instruments to clean and shape the inside of the tooth. The goal is to remove all remaining infection and debris to create a smooth, sterile environment.
- Sealing the Tooth: After cleaning the canal, the dentist will fill it with a rubber-like material called gutta-percha, which helps seal the tooth and prevent future infection. In many cases, the tooth will be temporarily sealed until a permanent crown or filling can be placed.
- Placement of the Final Restoration: After the root canal procedure is completed, the dentist will usually recommend placing a crown or filling on the tooth to restore its shape, strength, and functionality. A crown is particularly recommended for back teeth, which endure significant pressure from chewing.
Recovery After a Root Canal
The recovery process after a root canal is generally minimal, especially when compared to the pain people often associate with the procedure. Here’s what to expect after the treatment:
- Discomfort: Some mild discomfort or tenderness is normal for a few days after the procedure, especially if there was significant infection. Over-the-counter pain relievers like ibuprofen or acetaminophen are usually sufficient to manage the pain.
- Swelling and Bruising: Swelling around the treated area may occur, but it typically resolves within a few days. Cold compresses can help reduce swelling.
- Temporary Sensitivity: Your tooth may remain sensitive to pressure for a few weeks following the procedure, particularly if the infection was severe before the root canal. However, this sensitivity should gradually subside as the tooth heals.
- Follow-up Care: If a temporary filling was used, your dentist will schedule a follow-up appointment to place a permanent crown or filling. It’s important to follow your dentist’s instructions and attend these follow-up visits to ensure proper healing.
Potential Complications and Risks
While root canals are generally safe and effective, like any medical procedure, they do carry some risks. However, these risks are rare and can be minimized with proper care and attention. Potential complications include:
- Reinfection: If the tooth is not properly sealed, bacteria may enter the root canal and cause reinfection. This is why it’s essential to follow through with the permanent restoration (usually a crown) after the procedure.
- Fractured Tooth: In some cases, the treated tooth may become weaker and more prone to fracture. This is another reason why placing a crown over the tooth is important.
- Persistent Pain: Some patients may experience persistent pain or discomfort even after the root canal is completed. If this occurs, it could indicate an issue with the healing process or the need for additional treatment.
Alternatives to Root Canal Treatment
In cases where a tooth is severely damaged beyond repair, or if a root canal is not feasible, an extraction may be necessary. While tooth extraction removes the infected tooth, it can result in complications like shifting of surrounding teeth, bite problems, and difficulty chewing. After extraction, a dental implant, bridge, or partial denture may be needed to restore functionality.
Myths and Misconceptions About Root Canals
Many people fear root canals due to misconceptions. Let’s clear up a few myths:
- Myth 1: Root canals are painful – This is perhaps the most common myth. Thanks to modern anesthesia and advanced techniques, most root canals are no more painful than having a routine filling.
- Myth 2: Root canals are dangerous – Root canals are a safe procedure that preserves the tooth and prevents further infection. They are often less risky than tooth extractions, which can lead to further complications.
- Myth 3: Root canals are only for older people – Root canal treatments can be performed on patients of all ages, as long as the tooth is still viable. Both children and adults may require root canals for a variety of reasons.
Conclusion
Root canals are a safe, effective, and commonly performed procedure that can save a tooth and alleviate significant pain caused by infection or injury. With advances in dental techniques and anesthesia, root canals today are far more comfortable than many people believe. If you experience severe tooth pain, swelling, or sensitivity, it’s essential to see a dentist who can assess the situation and determine if a root canal is necessary. Early intervention can help prevent complications and keep your smile healthy for years to come.